Colon Cancer Surgery
Understanding the Surgical Approaches for Colon Cancer Treatment in Singapore
What is colon cancer?
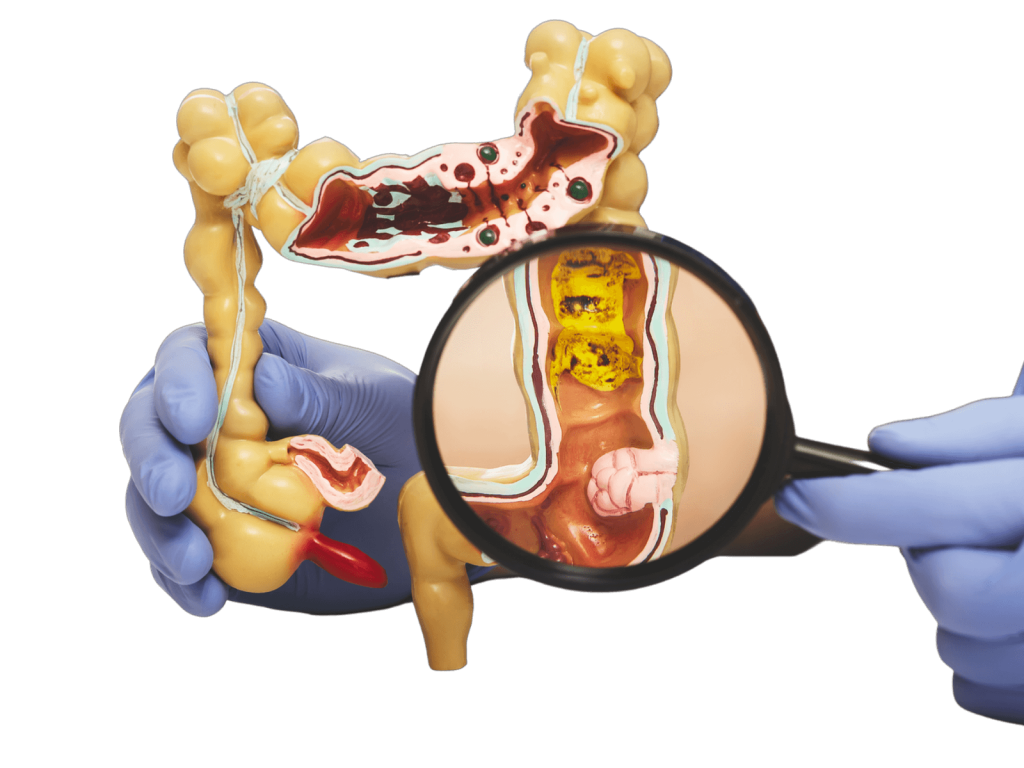
Colon cancer is a type of cancer that develops in the colon (large intestine). It usually starts as small, non-cancerous growths called polyps, which can become cancerous over time. Colon cancer is one of the most commonly diagnosed cancers worldwide including Singapore.
What are the common symptoms?
Common symptoms of colon cancer include:
- Changes in bowel habits, such as diarrhea or constipation, that last for more than a week.
- Blood in the stool or rectal bleeding
- Persistent abdominal pain, discomfort or bloating sensation
- Unexplained weight loss (not intentional diet)
- Change in stool caliber
- Anemia (low in red blood count)
What are the risk factors?
Some common risk factors for colon cancer include:
- Age (the risk of colorectal cancer increases after the age of 50)
- Personal or family history of colorectal cancer or polyps
- Inflammatory bowel disease (such as ulcerative colitis or Crohn’s disease)
- A diet high in red or processed meats and low in fruits and vegetables
- Smoking and tobacco use
- Certain inherited genetic syndromes, such as Lynch syndrome or familial adenomatous polyposis (FAP)
How to diagnose colon cancer?
Colonoscopy is considered the gold standard for diagnosing colon cancer due to its high accuracy and reliability. In addition to visual examination, your doctor may also take a small tissue sample (biopsy) from any suspicious areas for further examination under a microscope. Possible colon cancer can be confirmed with the biopsy.
After a diagnosis of colon cancer is confirmed, additional investigations may be conducted to determine the extent or stage of the cancer. These investigations may include:
Computed Tomography (CT) scan: This imaging test is commonly used to stage colon cancer. It provides detailed images of the colon and surrounding tissues, and can detect any local invasion or extension of the cancer, as well as any distant spread of the disease, such as to the liver or lungs.
Positron Emission Tomography (PET) scan: PET scan is an alternative staging test to CT scan for colon cancer. It is more sensitive in detecting metabolic activity of cancers, but it can produce false-positive results due to uptake of the tracer in non-cancerous tissues or inflammation.
Carcinoembryonic antigen (CEA) blood test: CEA is a protein that may be secreted by colon cancer into the bloodstream. However, not all colon cancers produce CEA, and other factors such as smoking or inflammation may also increase CEA levels. Therefore, CEA levels should be interpreted with caution.
What are the stages of colon cancer?
Colon cancer is classified into stages based on how advanced it is. There are four stages:
Stage I, the cancer has grown through the inner lining of the colon and into the middle layers but has not spread beyond the colon wall.
Stage II, the cancer has grown through the colon wall and may have invaded nearby tissues or organs but has not spread to the lymph nodes.
Stage III, the cancer has spread to nearby lymph nodes.
Stage IV, the cancer has spread to other parts of the body, such as the liver or lungs.
How to treat colon cancer?
 The approach to treating colon cancer is dependent on several factors, including the stage of the cancer, the patient’s age, overall health, and personal preferences. The three primary treatments for colon cancer are surgery, chemotherapy, and radiation therapy, each with its specific role.
The approach to treating colon cancer is dependent on several factors, including the stage of the cancer, the patient’s age, overall health, and personal preferences. The three primary treatments for colon cancer are surgery, chemotherapy, and radiation therapy, each with its specific role.
Surgery remains the most common treatment for colon cancer and aims to remove the cancerous tumor and the draining lymph nodes. It is the primary form of treatment for achieving a complete cure.
Chemotherapy, usually given after surgery to eliminate any remaining cancer cells. For advanced or metastatic colon cancer, chemotherapy may be used as the primary treatment.
Radiation therapy is infrequently used to treat curative colon cancer but may be employed to alleviate symptoms of advanced colon cancer, such as pain or bleeding.
 The approach to treating colon cancer is dependent on several factors, including the stage of the cancer, the patient’s age, overall health, and personal preferences. The three primary treatments for colon cancer are surgery, chemotherapy, and radiation therapy, each with its specific role.
The approach to treating colon cancer is dependent on several factors, including the stage of the cancer, the patient’s age, overall health, and personal preferences. The three primary treatments for colon cancer are surgery, chemotherapy, and radiation therapy, each with its specific role.
Surgery remains the most common treatment for colon cancer and aims to remove the cancerous tumor and the draining lymph nodes. It is the primary form of treatment for achieving a complete cure.
Chemotherapy, usually given after surgery to eliminate any remaining cancer cells. For advanced or metastatic colon cancer, chemotherapy may be used as the primary treatment.
Radiation therapy is infrequently used to treat curative colon cancer but may be employed to alleviate symptoms of advanced colon cancer, such as pain or bleeding.
What are the surgical approach for colon cancer?
Colon cancer surgery aims to remove the cancerous tumor and nearby lymph nodes while preserving healthy tissue and bowel function. Previously, open laparotomy via a long midline incision was the standard approach, but now minimally invasive laparoscopic surgery is more common. However, open surgery may still be necessary for specific patient groups, such as those with multiple previous surgeries or obstructed colon cancer.
Laparoscopy involves a few small incisions in the abdomen, resulting in less pain, faster recovery, and minimal blood loss. Robotic-assisted surgery, using the da Vinci system, may be utilized for more complicated cases, as it can enhance surgical precision.
Unlike in rectal surgery, elective colon surgery typically does not require the creation of a stoma or ostomy.
What are the potential complications of colon cancer surgery?
Colon cancer surgery is a significant procedure that carries some potential risks. Here are some of the possible complications:
- Bleeding: There is a risk of bleeding from the resection site or at the anastomosis.
- Infection: Patients undergoing colon cancer surgery are at risk of developing intra-abdominal infections and superficial wound infections.
- Anastomotic leak: The new connection between two ends of the bowel may not heal properly, leading to stool leakage into the abdomen. This is a serious complication that may require further surgery.
- Damage to nearby organs: During the surgery, there is a risk of accidentally damaging nearby organs, such as the bladder, ureter, or small intestine.
- Blood clots: There is a risk of developing blood clots, such as deep vein thrombosis (DVT), which can lead to more serious complications if the clots dislodge and travel to the lung, causing pulmonary embolism.
- Bowel obstruction: There is a risk of bowel adhesions forming after the surgery, which can lead to bowel obstruction in the future.
Book Appointment
Book your consultation today for expert surgical care.
