ANAL FISSURE SURGERY
What is anal fissure?
Anal fissure is a tear at the lower end of anus.
What are the symptoms?
- Anal pain especially during passing motion.
- Burning sensation or pain at anus lasting for several minutes after passing motion.
- Fresh bright red blood on surface of stool or on toilet paper
- Small lump at anus associated with pain.
What causes anal fissure?
Common causes of anal fissure are constipation, passing out large hard stool, straining, chronic diarrhoea and inflammatory bowel disease (IBD).
How to treat anal fissure?
- Anal fissures can be healed with conservative treatment
- Treatment goals: promote blood flow to the anus, alleviate pain, and soften stool
- Treatment methods:
- Dietary changes (high-fiber diet)
- Topical medications (ointment with lidocaine, hydrocortisone, nitroglycerin)
- Stool softeners (laxatives)
- Alternative treatments if conservative treatment fails:
- Botox injections (relax the muscles around the anus)
- Surgery (lateral anal sphincterotomy) to reduce pressure on the anal fissure and promote healing.
What you need to know about anal fissure surgery?
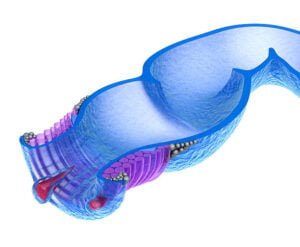
A lateral anal sphincterotomy (LAS) is the most common type of sphincterotomy used to treat anal fissures.
During a LAS, the surgeon will make a small incision in the internal anal sphincter muscle. This is the muscle that surrounds the anal canal and helps to control bowel movements. By cutting a small portion the muscle, the pressure on the anal fissure is reduced, which can help promote healing.
LAS is typically performed under general anesthesia. The surgery usually takes about 30 minutes to an hour and patient go home on the same day.
After the surgery, patients may experience some discomfort and soreness around the anus. Pain medication can be prescribed to help manage the discomfort. It’s important to follow post-operative care instructions closely to prevent complications and ensure proper healing. This may include taking stool softeners to prevent constipation, soaking in warm water baths (sitz baths), and avoiding heavy lifting or strenuous activities for several weeks after surgery.
What are the risk of anal fissure surgery?
Some of the potential risks include:
Infection: Infection can occur after any surgical procedure.
Bleeding: There may be some bleeding after surgery, but it is usually minimal and stops by itself.
Incontinence: The internal anal sphincter muscle is responsible for controlling bowel movements, and cutting it may result in temporary or permanent loss of control over bowel movements. This risk is low, but it’s important to discuss this potential complication with your doctor.
Pain: Pain is common after surgery, but it is usually manageable with pain medications.
Scar tissue: Scar tissue may form after surgery, which can potentially cause complications such as narrowing of the anal canal.
Overall, anal fissure surgery is safe and very effective treatment for anal fissure but its critical to discuss it with your surgeon before the procedure.

Other Colorectal Surgery
Consult Us

Dr LEE Kuok Chung
Senior Consultant General Surgeon
Subspeciality interest: Colorectal, Advanced Endoscopy and Robotic Surgery

Dr TAN Wee Boon
Senior Consultant General Surgeon
Subspeciality interest: Thyroid, Hernia and Endocrine Surgery

Dr KIM Guowei
Senior Consultant General Surgeon
Subspeciality interest: Upper Gastrointestinal, Bariatric and Robotic Surgery
Crest Surgical Practice
Healing Hands, Compassionate Hearts: Your Partner in Surgical Care

