COLON POLYPS
What is colon polyps?
Colon polyps are abnormal growths that form on the inner lining of the colon or rectum. These growths are usually benign but can sometimes turn cancerous over time.
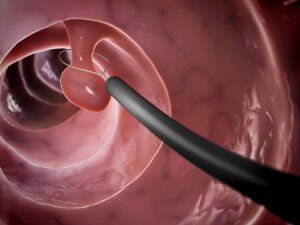
Colon polyps vary in size and shape and can appear as small, flat bumps or as larger, mushroom-shaped growths.
What causes colon polyps?
The exact causes of colon polyps are not fully understood, but certain factors have been identified that may increase the risk of developing them. These factors include:
Age: Colon polyps are more common in people over the age of 50.
Genetics: Individuals with a family history of colon polyps or colon cancer have a higher risk of developing colon polyps themselves.
Lifestyle factors: Certain lifestyle factors such as a diet high in fat and low in fiber, smoking, and sedentary behavior may increase the risk of developing colon polyps.
Medical conditions: Individuals with inflammatory bowel disease (IBD) such as ulcerative colitis or Crohn’s disease are at an increased risk of developing colon polyps.
What are the symptoms?
Colon polyps often do not cause any symptoms, which is why regular screening COLONOSCOPY is important for early detection and removal. However, some people may experience the following symptoms if the polyps grow large enough:
Rectal bleeding: This may appear as bright red blood on the toilet paper after a bowel movement or in the toilet bowl.
Changes in bowel habits: This may include diarrhea, constipation, or narrow stools that last for more than a few days.
Abdominal pain or cramping: This may be constant or come and go and may be accompanied by bloating.
Fatigue or weakness: This may be due to anemia caused by chronic rectal bleeding.
How to remove colon polyps?
The vast majority of colon polyps can be safely removed during a colonoscopy, particularly those under 1cm in size, which can be removed through polypectomy. However, for larger or more complex polyps, advanced methods such as endoscopic mucosal dissection (EMR) or endoscopic submucosal dissection (ESD) may be necessary. These techniques can be performed during the same colonoscopy, but more commonly, they are done later due to their longer duration and the need for pre-procedure preparation.
In some cases, very large polyps may be too risky to remove endoscopically, and surgery (colectomy) may be required.
Why surgery maybe done for colon polyps?
Indications for surgery in colon polyps include:
- Large polyps (usually >2cm) that cannot be safely removed endoscopically or failed EMR/ESD.
- Polyps (even complete polypectomy) that are suspicious for or have already developed into colon cancer.
- Polyps that have grown back after previous endoscopic removal attempts.
- Certain types of polyps that have a high risk of developing into cancer, such as serrated polyps with dysplasia or familial adenomatous polyposis (FAP).
Surgery may involve removal of a portion of the colon (partial colectomy) or the entire colon (total colectomy). The specific type of surgery will depend on the size, location, and features of the polyp, as well as the overall health of the patient.

Other Colorectal Surgery
Consult Us

Dr LEE Kuok Chung
Senior Consultant General Surgeon
Subspeciality interest: Colorectal, Advanced Endoscopy and Robotic Surgery

Dr TAN Wee Boon
Senior Consultant General Surgeon
Subspeciality interest: Thyroid, Hernia and Endocrine Surgery

Dr KIM Guowei
Senior Consultant General Surgeon
Subspeciality interest: Upper Gastrointestinal, Bariatric and Robotic Surgery
Crest Surgical Practice
Healing Hands, Compassionate Hearts: Your Partner in Surgical Care

