Colon Stenting
Understanding Colon Stenting: Procedure, Indications, and Benefits for Colon Health
What is a colon stent?
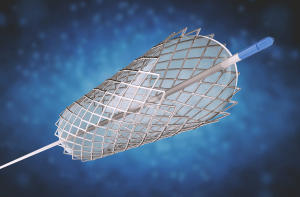
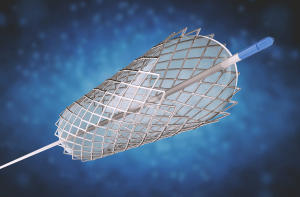
 A colon stent is a medical device designed to help relieve a blockage in the colon or rectum caused by cancer, inflammation, or other conditions. It is a small metal mesh tube that is placed inside the colon to keep the passageway open and allow stool to pass through.
A colon stent is a medical device designed to help relieve a blockage in the colon or rectum caused by cancer, inflammation, or other conditions. It is a small metal mesh tube that is placed inside the colon to keep the passageway open and allow stool to pass through.
The procedure to insert a colon stent is minimally invasive and typically done using a colonoscope, a thin, flexible tube with a camera and a light on the end. The colonoscope is passed through the rectum and into the colon, and the stent is placed in the blocked area. Once in place, the stent expands to keep the colon open and allows stools to pass through.
 A colon stent is a medical device designed to help relieve a blockage in the colon or rectum caused by cancer, inflammation, or other conditions. It is a small metal mesh tube that is placed inside the colon to keep the passageway open and allow stool to pass through.
A colon stent is a medical device designed to help relieve a blockage in the colon or rectum caused by cancer, inflammation, or other conditions. It is a small metal mesh tube that is placed inside the colon to keep the passageway open and allow stool to pass through.
The procedure to insert a colon stent is minimally invasive and typically done using a colonoscope, a thin, flexible tube with a camera and a light on the end. The colonoscope is passed through the rectum and into the colon, and the stent is placed in the blocked area. Once in place, the stent expands to keep the colon open and allows stools to pass through.
When is colon stenting done?
Common indication in the following situations:
Palliative treatment for advanced colon cancer: Patients with advanced colon cancer may experience a blockage in the colon or rectum, making it difficult to pass stool. Colon stenting can help relieve the blockage and improve the patient’s quality of life by avoiding stoma (ostomy) creation.
Preoperative preparation (general guideline): Colon stenting may be used as a bridge to surgery in some cases. For example, if a patient has a large tumor in the colon, stenting may be used to relieve the blockage and allow the patient to regain strength before undergoing surgery. This also allows possibility of minimally invasive (keyhole or laparoscopic surgery) to be carried out safely at later date.
What are the contraindications?
There are several contraindications to colon stenting, which include:
Colonic Perforation: Patients with perforation in the colon may not be candidates for colon stenting. In these cases, immediate surgery may be required.
Bleeding: Patients with active bleeding in the colon may not be candidates for colon stenting, as the procedure can increase the risk of bleeding.
Uncontrolled infection: Patients with uncontrolled infection may not be candidates for colon stenting, as the procedure can increase the risk of infection.
Anatomy: Patients with complex anatomy or abnormal anatomy in the colon may not be candidates for colon stenting, as it may be difficult to place the stent in the correct location.
Pregnancy: Pregnant patients may not be candidates for colon stenting, as the procedure involves radiation which can pose risks to both the mother and the fetus.
It is important to note that the decision to perform colon stenting depends on the patient’s individual condition. A qualified doctor will evaluate the patient and review any imaging studies to determine if colon stenting is appropriate.
What happens if colon stenting failed?
A failed stenting may include the need for emergency surgery, delayed treatment, increased risk of complication and, reduced quality of life.
What happens after successful colon stenting?
 For patients with resectable colon cancer, colon stenting may be used as a temporary measure to relieve the blockage and improve symptoms before undergoing elective surgery to remove the cancer. Elective surgery for resectable colon cancer typically involves removing the affected portion of the colon, along with nearby lymph nodes, to prevent the cancer from spreading to other parts of the body.
For patients with resectable colon cancer, colon stenting may be used as a temporary measure to relieve the blockage and improve symptoms before undergoing elective surgery to remove the cancer. Elective surgery for resectable colon cancer typically involves removing the affected portion of the colon, along with nearby lymph nodes, to prevent the cancer from spreading to other parts of the body.
The timing of elective surgery after colon stenting depends on several factors, including the stage of the cancer, the patient’s overall health, and the extent of the colon blockage. Usually your surgeon will aim to perform the surgery one to two weeks after the colon stenting.
During the period between colon stenting and elective surgery, patients may undergo additional imaging studies or other tests to monitor the progression of the cancer and ensure that the stent is functioning properly. In some cases, patients may receive chemotherapy or radiation therapy before surgery to shrink the tumour and improve the chances of a successful outcome.
 For patients with resectable colon cancer, colon stenting may be used as a temporary measure to relieve the blockage and improve symptoms before undergoing elective surgery to remove the cancer. Elective surgery for resectable colon cancer typically involves removing the affected portion of the colon, along with nearby lymph nodes, to prevent the cancer from spreading to other parts of the body.
For patients with resectable colon cancer, colon stenting may be used as a temporary measure to relieve the blockage and improve symptoms before undergoing elective surgery to remove the cancer. Elective surgery for resectable colon cancer typically involves removing the affected portion of the colon, along with nearby lymph nodes, to prevent the cancer from spreading to other parts of the body.
The timing of elective surgery after colon stenting depends on several factors, including the stage of the cancer, the patient’s overall health, and the extent of the colon blockage. Usually your surgeon will aim to perform the surgery one to two weeks after the colon stenting.
During the period between colon stenting and elective surgery, patients may undergo additional imaging studies or other tests to monitor the progression of the cancer and ensure that the stent is functioning properly. In some cases, patients may receive chemotherapy or radiation therapy before surgery to shrink the tumour and improve the chances of a successful outcome.
Book Appointment
Book your consultation today for expert surgical care.
