Inguinal Hernia Surgery
Understanding Inguinal Hernia Surgery: Treatment Options and Recovery
What is a hernia?
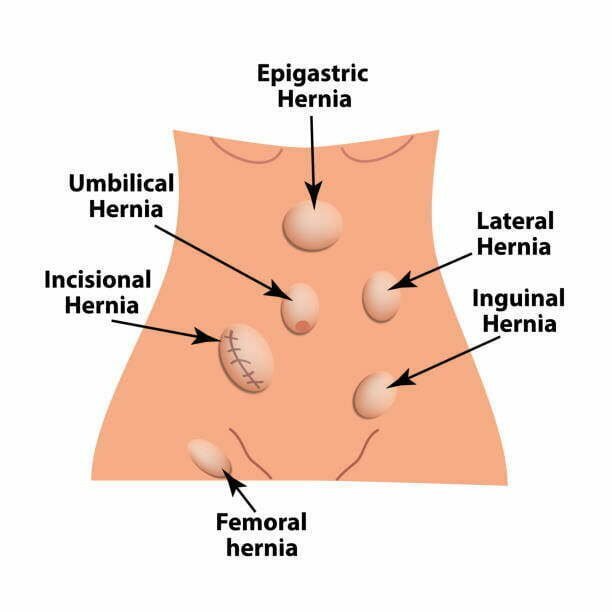
A hernia refers to the protrusion of abdominal fat or organs, such as the intestine, through a weakened area or opening in the abdominal muscles. This condition affects both men and women and its incidence typically increases with age. Hernias are classified according to their location on the body.
The two types of groin hernias are inguinal and femoral, with the former being more common. Femoral hernias, on the other hand, occur more frequently in women and may cause more acute symptoms.
How do you know if you have an inguinal hernia?
- Inguinal hernias may cause various symptoms, such as a bulge or swelling in the groin that worsens with standing and improves when lying down.
- Pain or discomfort over the hernia, especially during physical activity or straining, is also common.
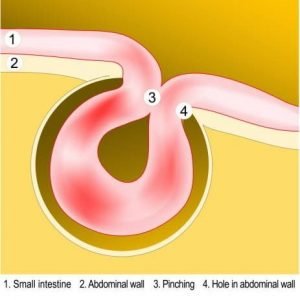
- Trapping of the herniated tissue may occur, causing blockage of the intestine, severe pain, vomiting, and abdominal distension.
- Strangulation is a rare but serious complication that requires emergency surgery, with an estimated risk of around 3% per year.
- Some patients may be asymptomatic, and hernias may be detected incidentally on imaging studies.
- Diagnosis is typically made through physical examination, although imaging (Ultrasound or CT scan) may be needed in complex cases.
Who are at risk of developing a hernia?
- Older patients
- Constant heavy lifting/strenuous physical activity
- Chronic cough such as asthma
- Chronic straining due to constipation or passing urine
- Obesity
- Pregnancy
How is hernia treated?
 The majority of hernias require surgical intervention to alleviate symptoms and prevent complications such as strangulation. Left untreated, the hernia will gradually increase in size over time. Following a thorough examination, your surgeon will determine whether a laparoscopic (keyhole) or an open inguinal hernia repair is the most suitable option for you. Typically, a surgical prosthesis (mesh) is employed to fortify the weakened region of the abdominal wall.
The majority of hernias require surgical intervention to alleviate symptoms and prevent complications such as strangulation. Left untreated, the hernia will gradually increase in size over time. Following a thorough examination, your surgeon will determine whether a laparoscopic (keyhole) or an open inguinal hernia repair is the most suitable option for you. Typically, a surgical prosthesis (mesh) is employed to fortify the weakened region of the abdominal wall.
The procedure is commonly performed under general anesthesia, although spinal anesthesia or local anesthesia with sedation may be utilized in select cases.
 The majority of hernias require surgical intervention to alleviate symptoms and prevent complications such as strangulation. Left untreated, the hernia will gradually increase in size over time. Following a thorough examination, your surgeon will determine whether a laparoscopic (keyhole) or an open inguinal hernia repair is the most suitable option for you. Typically, a surgical prosthesis (mesh) is employed to fortify the weakened region of the abdominal wall.
The majority of hernias require surgical intervention to alleviate symptoms and prevent complications such as strangulation. Left untreated, the hernia will gradually increase in size over time. Following a thorough examination, your surgeon will determine whether a laparoscopic (keyhole) or an open inguinal hernia repair is the most suitable option for you. Typically, a surgical prosthesis (mesh) is employed to fortify the weakened region of the abdominal wall.
The procedure is commonly performed under general anesthesia, although spinal anesthesia or local anesthesia with sedation may be utilized in select cases.
What you need to know about inguinal hernia surgery?
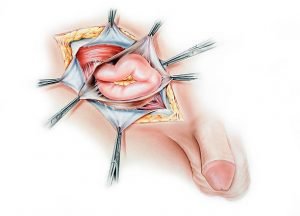
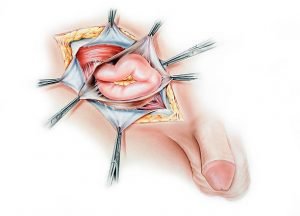
This is done from outside through a 6-8cm incision in the groin. The wound is deepened to the muscle layer and the surgeon then reduces the bulge and repair the weakened area with a mesh. Sutures are typically used to hold the mesh in place.
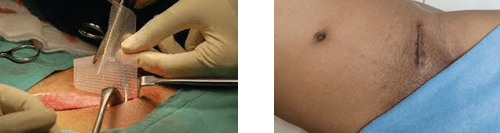
In laparoscopic hernia surgery, a laparoscope (tiny camera) is used for visualisation. This is usually inserted near the umbilicus. The hernia is reduced using laparoscopic instruments and a mesh is placed and held in place by absorbable tackers.
Advantages of keyhole surgery:
- Smaller wounds, less pain, faster return to usual activities.
- Hernias on both sides can be repaired using the same incisions in the midline.
- Better option to repair a recurrent hernia after a previous open surgery.

What preparation is required for inguinal hernia surgery?
Depending on your medical conditions, pre-operative preparations may include:
- Blood tests
- Chest X ray
- Electrocardiogram (ECG)
You will need to fast the night before the operation, but continue to take essential medications e.g., anti-hypertensive as instructed by your surgeon. You will also be asked to stop blood thinning medications like aspirin or a week before the surgery.
What should you expect after inguinal hernia surgery?
 Most patients are discharged on the same day of surgery or the day after. You will be able to leave the hospital once you are fully awake, ambulatory, able to tolerate solid food, and able to urinate. You may experience some soreness in the groin area, but this can be easily managed with painkillers that will be prescribed to you. Most patients are able to resume their normal daily activities within the first week following surgery. However, you should avoid strenuous activities such as heavy lifting for the next few weeks until your surgeon gives you permission to do so.
Most patients are discharged on the same day of surgery or the day after. You will be able to leave the hospital once you are fully awake, ambulatory, able to tolerate solid food, and able to urinate. You may experience some soreness in the groin area, but this can be easily managed with painkillers that will be prescribed to you. Most patients are able to resume their normal daily activities within the first week following surgery. However, you should avoid strenuous activities such as heavy lifting for the next few weeks until your surgeon gives you permission to do so.
You will have a follow-up appointment in the clinic 1 to 2 weeks after the surgery to review your wound and any symptoms. If you experience persistent fever, worsening abdominal pain with nausea and vomiting, or any problems with your wound such as swelling, bleeding, or discharge, please contact your surgeon immediately.
 Most patients are discharged on the same day of surgery or the day after. You will be able to leave the hospital once you are fully awake, ambulatory, able to tolerate solid food, and able to urinate. You may experience some soreness in the groin area, but this can be easily managed with painkillers that will be prescribed to you. Most patients are able to resume their normal daily activities within the first week following surgery. However, you should avoid strenuous activities such as heavy lifting for the next few weeks until your surgeon gives you permission to do so.
Most patients are discharged on the same day of surgery or the day after. You will be able to leave the hospital once you are fully awake, ambulatory, able to tolerate solid food, and able to urinate. You may experience some soreness in the groin area, but this can be easily managed with painkillers that will be prescribed to you. Most patients are able to resume their normal daily activities within the first week following surgery. However, you should avoid strenuous activities such as heavy lifting for the next few weeks until your surgeon gives you permission to do so.
You will have a follow-up appointment in the clinic 1 to 2 weeks after the surgery to review your wound and any symptoms. If you experience persistent fever, worsening abdominal pain with nausea and vomiting, or any problems with your wound such as swelling, bleeding, or discharge, please contact your surgeon immediately.
Book Appointment
Book your consultation today for expert surgical care.
